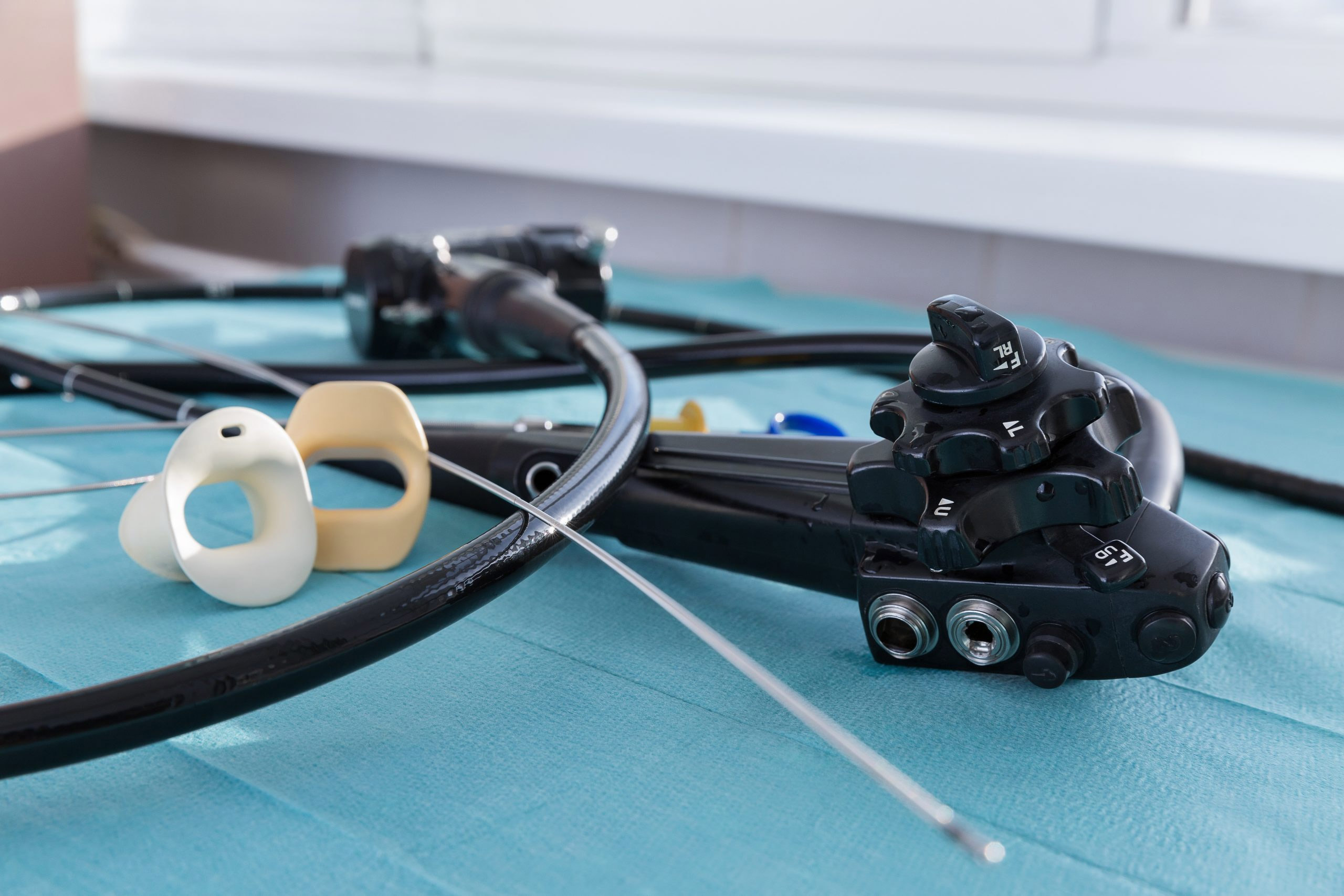
Cross-contamination of endoscopes has been one of the top health technology hazards for hospitals for eight years running, according to analysis published by patient safety researcher ECRI Institute.1 In fact, the number of medical device reports submitted to the U.S. Food and Drug Administration (FDA) on infection or device contamination associated with reprocessed flexible bronchoscopes hit an all-time high (183) in 2016, the most recently tracked timespan.2
The FDA identifies reusable bronchoscopes as posing a greater likelihood of microbial transmission and higher risk of infection if not properly reprocessed.3
At the same time, such reprocessing requires more than 100 steps per device, making it a costly, time-consuming and resource-intensive process. A pilot project focused on measuring the true cost of reprocessing found it to range from approximately $114 to $281 per endoscope, while requiring about 76 minutes of hands-on staff time. Additionally, the pilot study report concludes that its findings “likely underestimate the time and cost associated with endoscope reprocessing.”4
Aside from significant costs, hospitals that reuse endoscopes must also consider the cross-contamination risk that persists even after thorough cleaning and disinfection. A variety of scientific studies reveal the following conclusions:
A 2017 study assessed the cost-effectiveness of single-use flexible video bronchoscopes vs. reusable bronchoscopes. The single-use products carried an average cost per use $305, compared to $424 for the reusable instruments. In addition to the $119 per procedure estimated savings, reusable scopes held a 0.7 percent risk of infection, whereas single-use scopes, provided in sterile packaging, had no risk of infection.10
Separate research, also published in 2017, indicated that senior-level bronchoscopists achieved greater broncho alveolar lavage (BAL) volume with single-use flexible bronchoscopes than conventional bronchoscopes. “The greater BAL volume return achieved with single-use bronchoscopes could lead to reduced risk of post-procedural side effects such as cough, pleuritic chest pain and fever, which may improve tolerability and participant comfort,” according to the study report.11
Reusable bronchoscopes must go through pre-cleaning, transportation, leak testing, manual cleaning and rinsing, high-level disinfection, re-rinsing, drying and storage before each procedure. In addition, they can easily be damaged, with an average cost per repair of $3,259. The combination of capital investment, repair and reprocessing results in a $314 per-procedure cost burden.12
Also significant, reusable bronchoscopes may not always be available due to the cleaning/disinfecting regimen, whereas disposable scopes are always ready for use straight from the sterile packaging. Delays are costly in all departments of the hospital, but particularly so in surgery, where interruptions rack up at a rate of $35 per minute.13
All told, disposable bronchoscopes make a solid financial investment while taking risk of infection out of the patient safety equation.
1. Top 10 health technology hazards for 2018. ECRI Institute. Accessed December 10, 2017.
2. Manufacturer and User Facility Device Experience database. U.S. Food and Drug Administration. https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfmaude/search.cfm Accessed December 10, 2017.
3. Reprocessing medical devices in health care settings: Validation methods and labeling. U.S. Food and Drug Administration. https://www.fda.gov/downloads/medicaldevices/deviceregulationandguidance/guidancedocuments/ucm253010.pdf Accessed December 10, 2017.
4. A glimpse at the true cost of reprocessing endoscopes. International Journal of Healthcare Central Service Material Management. https://www.bostonscientific.com/content/dam/bostonscientific/uro-wh/portfolio-group/LithoVue/pdfs/Sterilization-Resource-Handout.pdf Accessed December 10, 2017.
5. Outbreak of pulmonary Pseudomonas aeruginosa and Stenotrophomonas maltophilia infections related to contaminated bronchoscope suction valves. Eurosurveillance. Volume 21, Issue 28. July 14, 2016.
6. Transmission of infection by flexible gastrointestinal endoscopy and bronchoscopy. Clinical Microbiology Review. Volume 26, No. 2. April 2013.
7. Transmission of multidrug-resistant organisms and other pathogens via contaminated endoscopes. Ofstead & Associates. 2013.
8. Microbiological monitoring of flexible bronchoscopes after high-level disinfection and flushing channels with alcohol: Results and costs. Respiratory Medicine. Volume 109, Issue 8. August 2015.
9. Practical toolkit for monitoring endoscope reprocessing effectiveness: Identification of viable bacteria on gastroscopes, colonoscopies and bronchoscopes. American Journal of Infection Control. Volume 44, Issue 7. July 1, 2016.
10. Early assessment of the likely cost-effectiveness of single-use flexible video bronchoscopes. PharmacoEconomics. 2017.
11. Single use and conventional bronchoscopes for Broncho alveolar lavage in research: A comparative study. BMC Pulmonary Medicine. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5420119/ Accessed December 11, 2017.
12. The aScope cost map (video). Ambu. https://www.ambu.com/products/flexible-endoscopes/bronchoscopes/product/ambu-ascope-4-slim Accessed December 11, 2017.
13. Ibid.
![]()