Physician assistants (PAs) are proving their worth in otolaryngology as retirement and burnout continue to claim large numbers of seasoned otolaryngologists each year.
The physician assistant designation came about in the 1960s to support primary care doctors but it has become a mainstay in a range of specialties, including otolaryngology.
“PAs represent an excellent opportunity to provide quality clinical patient care in a cost-effective manner, improving patient access to otolaryngology while providing ancillary revenue and profitability to an otolaryngology practice,” Dr. Gavin Setzen, from Albany ENT and Allergy Services in New York, said in an interview with ENT Today.
About 300 otolaryngology residents and fellows graduate each year, and given retirements and other departures, demand outpaces supply, Setzen added.
The role of PAs in otolaryngology can include working in an outpatient clinic with their own patient schedule, running independent clinics, assisting in operating rooms and serving on call for inpatient and emergency room consults.
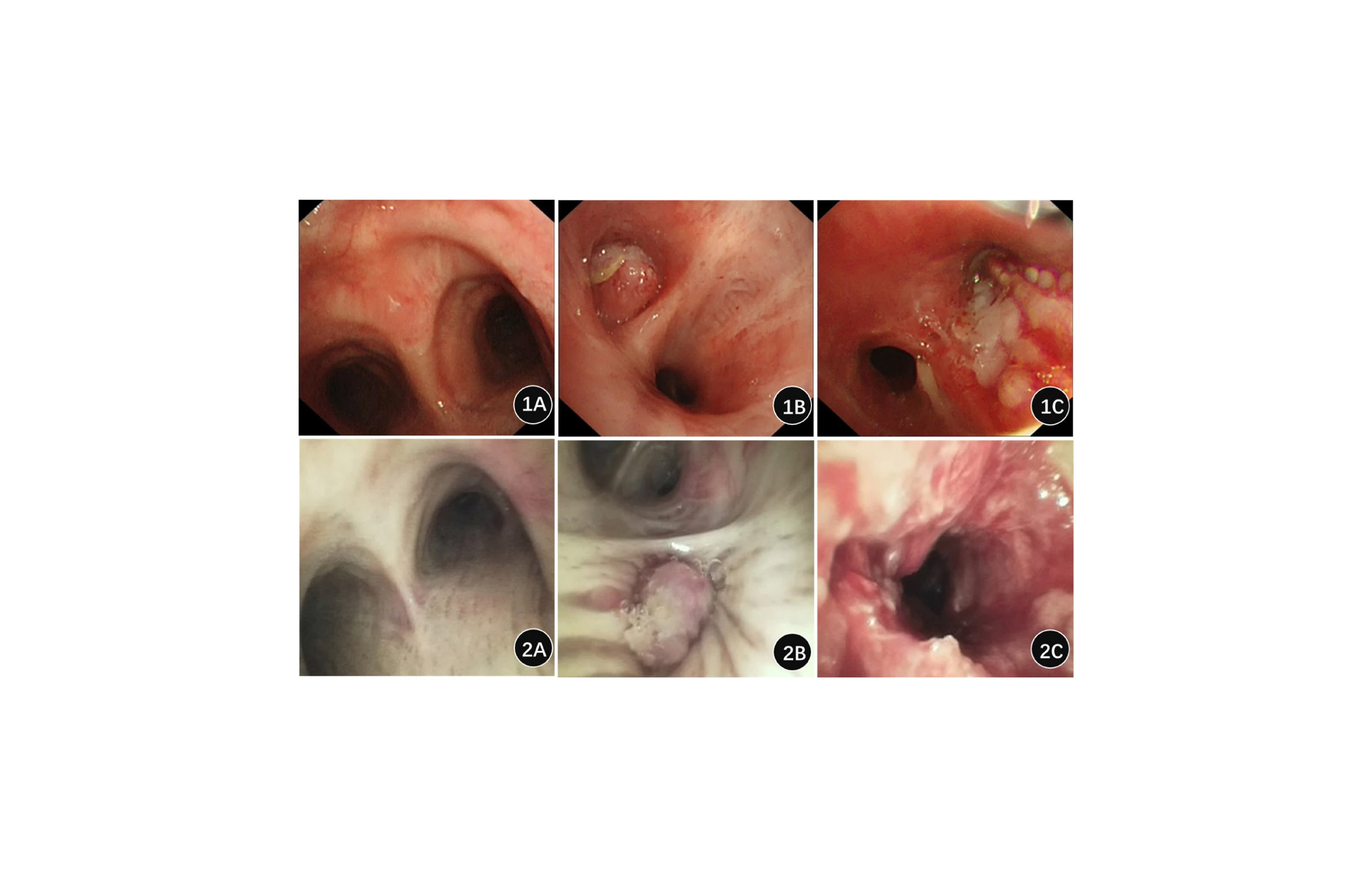
A recent survey reported that procedures performed by PAs in otolaryngology included: nasal endoscopy, fiberoptic laryngoscopy, foreign body removal, pre-op history and physical, excision/biopsy of lesions, and post-op debridement. That’s according to an issue brief created by the American Academy of Physician Assistants.
Educational programs for PAs require taking part in inpatient and outpatient rotations, including all core clinical settings plus electives. They also must complete a master’s thesis. The typical program takes about three years, after which they must pass the Physician Assistant National Certifying Exam.
When they hire a PA, some otolaryngology practices supplement the general coursework with various periods of on-the-job training to help ensure a successful transition into the workplace.
A well-trained PA can solve many challenges for a practice, Dr. John Carter, a pediatric otolaryngologist at Ochsner Health in Louisiana, told ENT Today.
“If your bottleneck is patient access, for example, your goal is to see more patients, and PAs are very helpful in expanding patient access,” Carter said. “Similarly, if you’re struggling with surgical conversion rates, a PA can by help by managing more of your nonsurgical or pre- and postop visits.”