Medicare is penalizing nearly 2,300 U.S. hospitals for having too many readmissions — a number that’s lower than it’s been since fiscal 2014, according to a recent analysis.
The federal government has eased its penalties as a result of the chaos caused by the COVID-19 pandemic, punishing just 2,273 hospitals in its recent assessment, the analysis by Kaiser Health News (KHN) found.
The Centers for Medicare & Medicaid Services decided to exclude the first half of 2020 in its annual calculation of the previous three years of readmissions because of the spike caused by the novel coronavirus pandemic. CMS also excluded Medicare patients readmitted with pneumonia during all three years because they are difficult to distinguish from patients with COVID-19.
Even given those adjustments, 43 percent of the 5,236 U.S. hospitals were penalized. Of those not penalized, all but 770 were automatically exempted. The 2,193 exempted hospitals include those that specialize in psychiatric patients, children or veterans, according to KHN. Rehabilitation and long-term care hospitals also are excluded.
The average payment reduction was .43 percent, which like the penalty numbers, was the lowest since 2014. Payment reductions will be applied to Medicare payments of the impacted hospitals from Oct. 1, 2022, through September 2023 and will cost $320 million over those 12 months.
Lowering readmission rates remains a national priority for payers, providers and policymakers seeking to improve healthcare while reducing costs.
The Hospital Readmissions Reduction Program was created in 2010 as part of the Affordable Care Act. The program measures how frequently Medicare patients return to hospitals within 30 days of their initial treatment and lowers future payments to hospitals that have higher-than-expected rates of readmissions.
Some hospitals have implemented new strategies to limit penalties by keeping patients from needing return visits. One strategy is setting up next-day appointments for patients who return to the emergency room within 30 days rather than readmitting them. Another is to call discharged patients to ensure that they have filled prescriptions and had a follow-up visit with a clinician within a week of leaving the hospital.
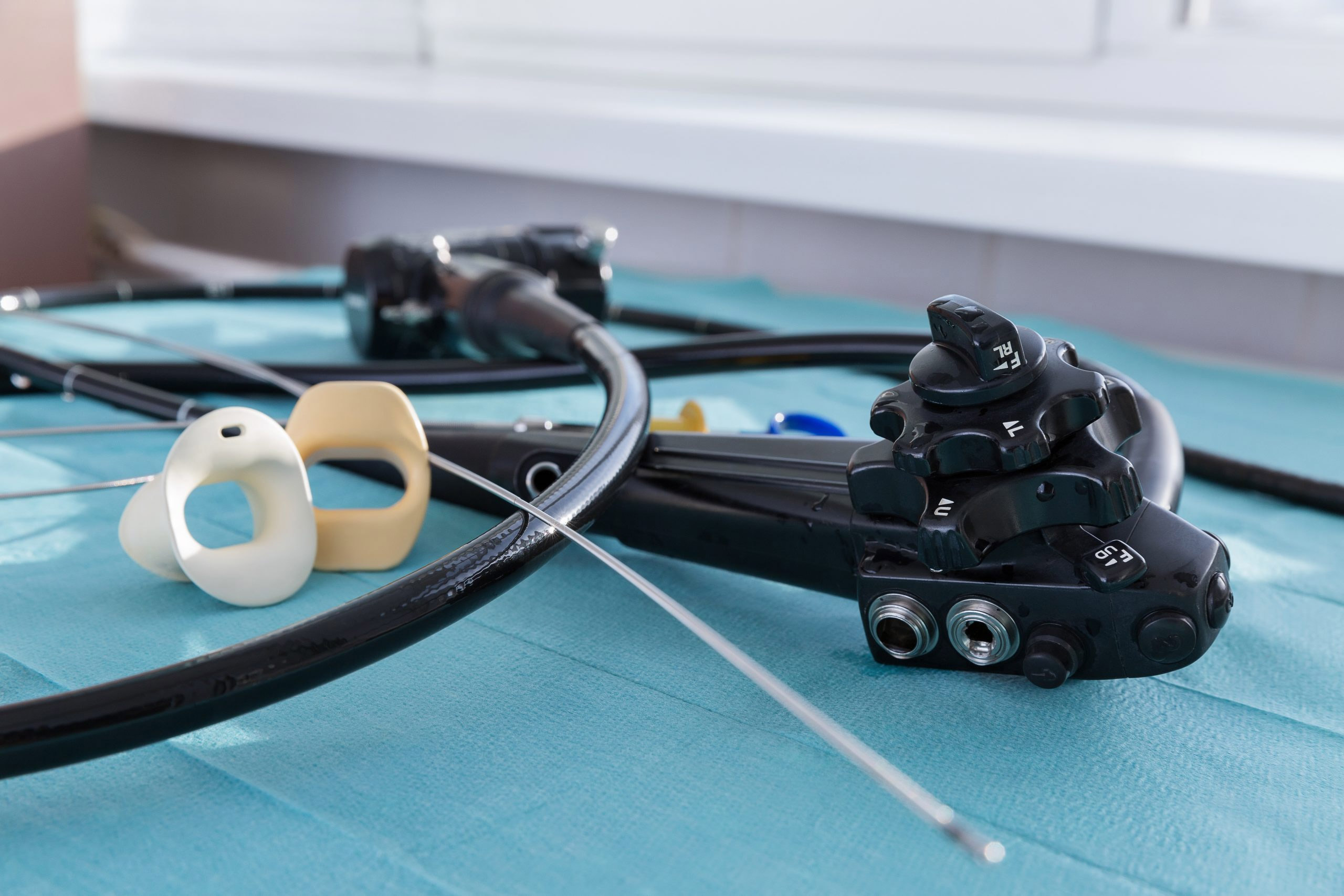
An abstract presented at the CHEST 2021 annual meeting showed that readmission rates can be reduced by more than half, and costs potentially lowered, by adopting single-use flexible bronchoscopes.
That study — by Dr. Hudson Garrett, an infection prevention specialist and an Ambu consultant — looked at the health outcomes of 14,228 patients who underwent a bronchoscopy and found that single-use bronchoscopes reduced the readmissions rate 53 percent, from 7.7 percent to 3.6 percent, compared with reusables.
His study followed a safety communication update from the U.S. Food and Drug Administration on reprocessing flexible bronchoscopes. The agency recommends that healthcare providers consider single-use bronchoscopes when there is increased risk of infection and when treating COVID-19 patients.
Last year, at the end of a decade of federal oversight of hospital readmissions, Medicare levied penalties on nearly half the nation’s hospitals in the form of reduced payments due to excessive revisits.
The average penalty was a .64 percent reduction per Medicare patient stay from October 2021 through September 2022, according to an earlier analysis by KHN. Those fines averaged $217,000 for a hospital in 2018, according to a congressional commission.
In the 2021 assessment, the maximum penalty, 3 percent, was imposed on 39 hospitals, while 547 hospitals saw so few readmissions that they received no penalty. Payments were reduced to 2,499 hospitals, or 47 percent of all U.S. facilities.