A new, artificial intelligence-based technology outperformed even “expert urologists” with more than 20 years of experience in terms of sensitivity to detect carcinoma in situ and small tumors in cystoscopic imaging.
The Cystoscopy Artificial Intelligence Diagnostic System (CAIDS) performed “exceptionally well” when rated on sensitivity, specificity, negative predictive value, and positive predictive value. The technology also enhanced the urologist’s ability to differentiate tumors from inflammatory changes. A recent editorial in the Journal of the National Cancer Institute analyzed the findings of a study published in the same issue.
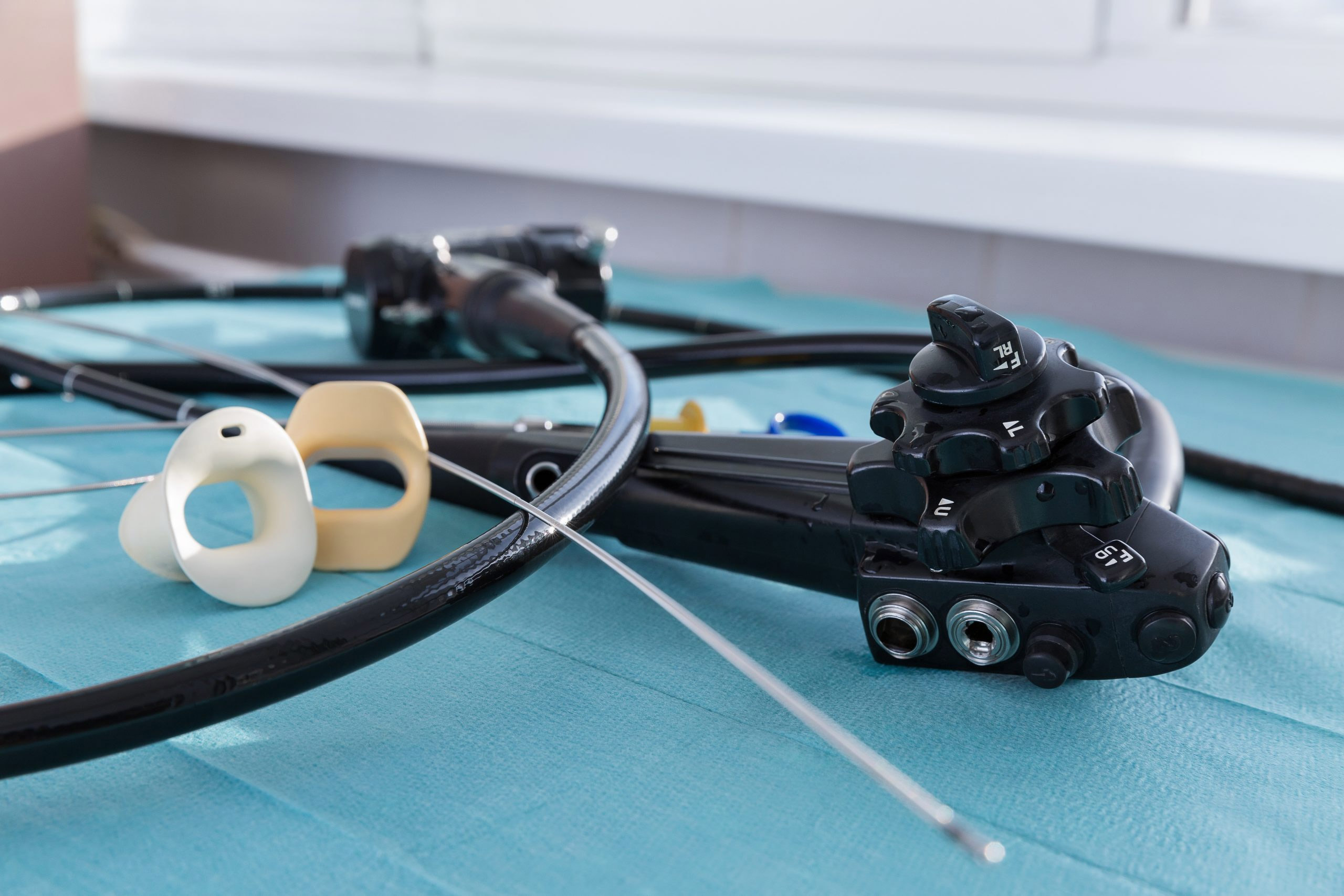
The AI system was trained on nearly 70,000 cystoscopic images taken from more than 10,000 patients. The images came from patients undergoing cystoscopy for possible bladder cancer or for surveillance after already having had it. Images were classified as either “tumor” or “normal” and were processed within 50 milliseconds. CAIDS can be integrated with standard equipment to use for diagnosis or treatment.
The editorial’s authors, Dr. Andrew T. Lenis of Memorial Sloan Kettering Cancer Center and Dr. Mark S. Litwin from the UCLA urology department, write that despite producing impressive results in recognizing cancerous images, urologists need to better understand CAIDS’ impact on outcomes for those with bladder cancer.
“Although the study clearly demonstrates an improvement in the accuracy and diagnostic capabilities of CAIDS over urologists of varying experience, this was not linked to the important endpoints in bladder cancer, namely, recurrence and progression,” they write. “CAIDS may identify a small low-risk lesion several months earlier than standard cystoscopy; however, this is unlikely to impact the patient’s ultimate quantity or quality of life.”
The invasive treatment required, and its high rate of recurrence, make bladder cancer one of the most expensive cancers to treat. Adding enhanced techniques such as CAIDS may increase cost without clinical benefit, the authors write.
“On the other hand, intermediate- and high-risk, nonmuscle-invasive tumors carry substantial risk of progression to invasive disease, and identification of additional tumors may well capture those who need more aggressive therapy,” they conclude.