A late June storm in Southeast Michigan saw peak winds estimated at 120 miles per hour, according to the National Weather Service. Between three and five inches of rain fell in the Detroit metro area. Nearby Wayne County was among the area’s hardest hit.
The storm that flooded thousands of homes also caused severe damage to Henry Ford Medical Center – Fairlane, in Dearborn. The Henry Ford Health System satellite endured flooding and damaged drywall. Its patients and doctors, including Dr. Craig Rogers, a urologist, were forced to relocate to a downtown Detroit hospital for more than two months.
What happened next is a testament to the power of new technology at a time when healthcare systems find themselves challenged on several fronts — clinical, financial, supply chain and logistics, even staffing.
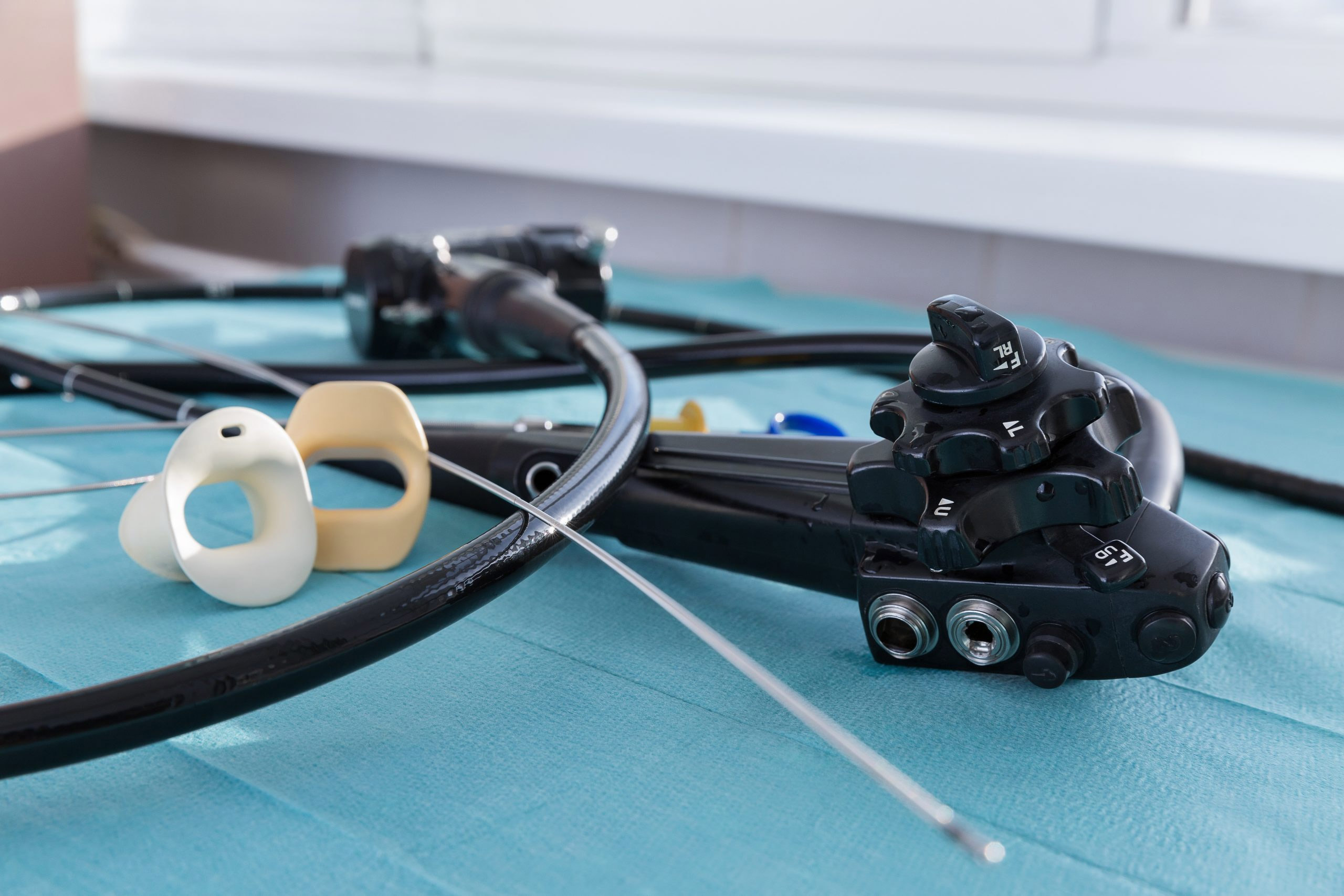
“We had to pivot on a dime and take all those patients that were coming in for clinic appointments and procedures and push them all to the downtown Detroit campus,” Rogers said. “There was no way we could just add on 30-plus cystoscopies a week to what we were already doing, in terms of reprocessing scopes and all that.”
To account for the additional patients and procedures, regular hospital rooms became exam rooms and cystoscopies were done with the single-use Ambu aScope 4 Cysto, which required fewer resources and staff to prepare.
"We were out of action in that clinic, sort of homeless per se. And during that time, the Ambu [cystoscope] totally saved us. We were able to salvage all those cystoscopies,” Rogers said. “We started turning regular rooms into exam rooms for cystoscopies and it worked fine.”
Though Fairlane is a smaller satellite within the Henry Ford Health System, dropping its roughly 30 cystoscopies per week would have resulted in a huge revenue hit — at a time when healthcare finances are already under strain thanks to COVID-19 and other factors.
And the displacement caused by the storm came toward the beginning of a separate crisis. Henry Ford — like countless other healthcare systems and businesses across all industries — found itself amid a staffing shortage brought on by the ongoing novel coronavirus pandemic. Rogers said his facility was short on nurses and medical assistants — the staff needed to run down a patient-ready scope or to reprocess the instruments after use was lacking.
“Probably everyone has felt the pinch sometimes where they don't have staffing. Or in a pinch, if you've got a patient you want to add on and they've driven a hundred miles to see you and they need a scope, do you really want to make him come back a week later to get a cystoscopy?” Rogers said. “Just because your procedure rooms are full and you don't have a little staffing that day, you need to accommodate that one patient. The Ambu scopes allow you to do that. When these cases come up, where you really need to accommodate someone and there's just no bandwidth, then you have that flexibility.”
Reusable cystoscopes require a tower and light source that needs to be plugged in. In the small exam rooms serving as makeshift procedure rooms, space became a limiting factor, Rogers explained. Additionally, the limited towers were already accounted for — assigned to procedure rooms where they remained.
Fortunately, Henry Ford had already begun incorporating single-use cystoscopes into practice about a year before staffing shortages took hold and flooding forced an entire clinic out of its facility.
One big reason was Henry Ford’s expansion.
“We were now expanding to places like Fairlane, Lakeside, Wyandotte. We're opening up these new ambulatory surgery centers. Bloomfield Township, for example, had just opened up,” Rogers said. “It's super expensive to just duplicate your capital every single place and say, ‘Alright, we're going to throw down another a hundred grand for a bunch of reusable scopes and towers.’”
Instead, Rogers and his colleagues decided on how to get up and running quickly at many sites at once.
“We just said, 'Look, we're not even going to deal with processing scopes. We're not even going to buy the towers,’” he said. “We don't have a place to process them anyway. Those scopes have to be shipped to another site for processing.
“That’s why we originally went with Ambu,” Rogers added. “We saw this as a way to facilitate an expansion strategy of our department — but then when a crisis happened, that was already in place as a potential solution.”