The Society of Urologic Nurses and Associates (SUNA) is celebrating those healthcare workers the week of Nov. 1-7 for their work with patients of all ages, in a variety of settings – and their dedication to patient safety is in the spotlight like never before thanks to the COVID-19 pandemic.
Urology nurses and associates have jobs that require not only a deep wellspring of clinical skills. They also perform their work with high levels of compassion and discretion due to the sometimes uncomfortable topics they must help patients navigate.
“Urology nurses and associates deserve the highest recognition for their amazing contributions and never-ceasing commitment to their patients,” said Amy Hull, president of the Society of Urologic Nurses and Associates in a letter to celebrate Urology Nurses and Associates Week. “Urology healthcare professionals treat men, women and children who experience a variety of urologic diseases and conditions, and these experts are highly adept at providing guidance and treatment to patients who often require complicated sub-specialty care.”
Here’s a list of frequently asked questions about these professionals and the important work they do.
What do urology nurses do?
Urology is a broad term, and urology nurses can specialize in any of a dozen practice areas to assist patients and medical staff with problems related to the urinary tract and reproductive organs and processes. These professionals administer tests, document vital signs, participate in check-ups, assist with surgeries, and diagnose and treat problems such as infections, kidney stones and cancer. They also educate patients and their families on illnesses, expectations for recovery and prevention measures.
Who are their patients?
Urology nurses may work with specific age groups or genders or help with patients of all ages and categories who need care for urological issues such as prostrate problems, kidney stones, incontinence and reproductive problems. They share many of the same responsibilities as medical staff, and because of their expertise and knowledge, often work independently or under minimal supervision.
Where do urology nurses work?
Urology nurses are found in hospitals, fertility centers, outpatient facilities and doctors’ offices. They may assist medical staff outside of urology, sometimes helping surgeons, intensive care workers and cancer specialists with procedures including biopsies, catheter insertions and scans. In the case of pediatric urology, they may also work closely with pediatric staff.
What are their biggest challenges?
Urology nurses help treat patients who may feel uncomfortable or embarrassed about their symptoms. That means nurses must be skilled at making people feel at ease discussing uncomfortable topics maturely. They also need to be observant so they can identify patient problems from sometimes vague descriptions. Being compassionate and discreet are key job requirements.
What are the education requirements to be a urology nurse?
Requirements vary by location and credential type, but a nursing certification such as a licensed practical nurse or nurse practitioner is needed. Individual states may require specific education or field work for these certificates.
What innovations are occurring in the field?
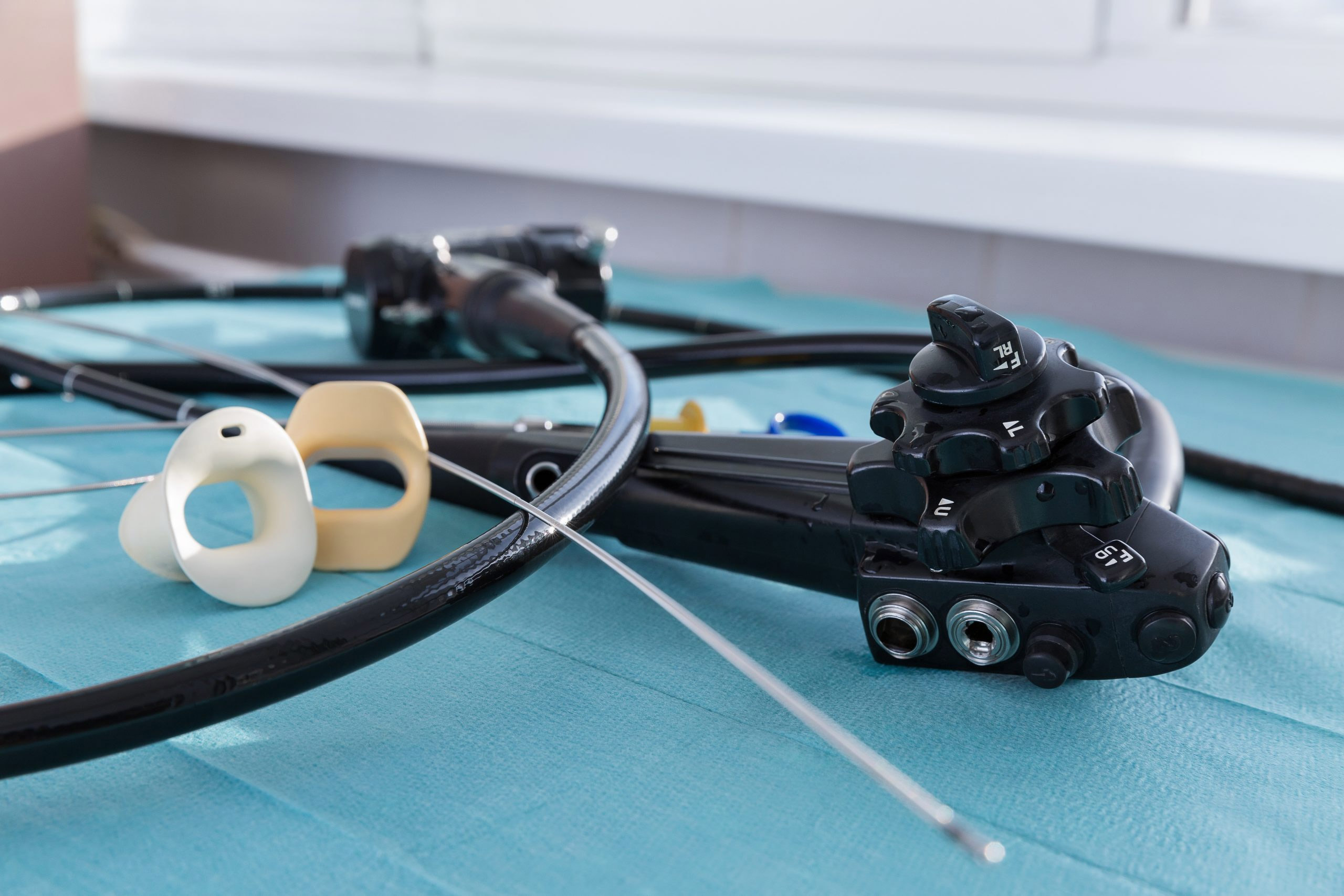
Among the innovations and new technology in the field are advances in laparoscopy, robotic surgery and digital imaging that offer increased precision. Telesurgery enables surgeons at remote locations to be trained by videoconferencing. There are new forms of cryosurgery (using a local application of intense cold to destroy unwanted tissue), while brachytherapy uses radioactive “seed” implants to help patients with low-grade tumors.
A recent meeting of the European Association of Urology Nurses included such agenda topics as ephrostomy care, catheter troubleshooting, bladder irrigation, manual washouts, uroflowmetry, bladder scanning, stoma care and flexible cystoscopy.