An investigation into a cluster of suspected Burkholderia cepacia complex infections among outpatients undergoing urologic procedures at a Kentucky regional acute care center in late 2020 led to several corrections in practices meant to prevent cross-contamination.
An internal probe of the outbreak found five cases that were epidemiologically linked through location, procedure, and/or staff between Jan. 22 and Oct. 8 of 2020. The findings and resolutions of the investigation were detailed in the American Journal of Infection Control.
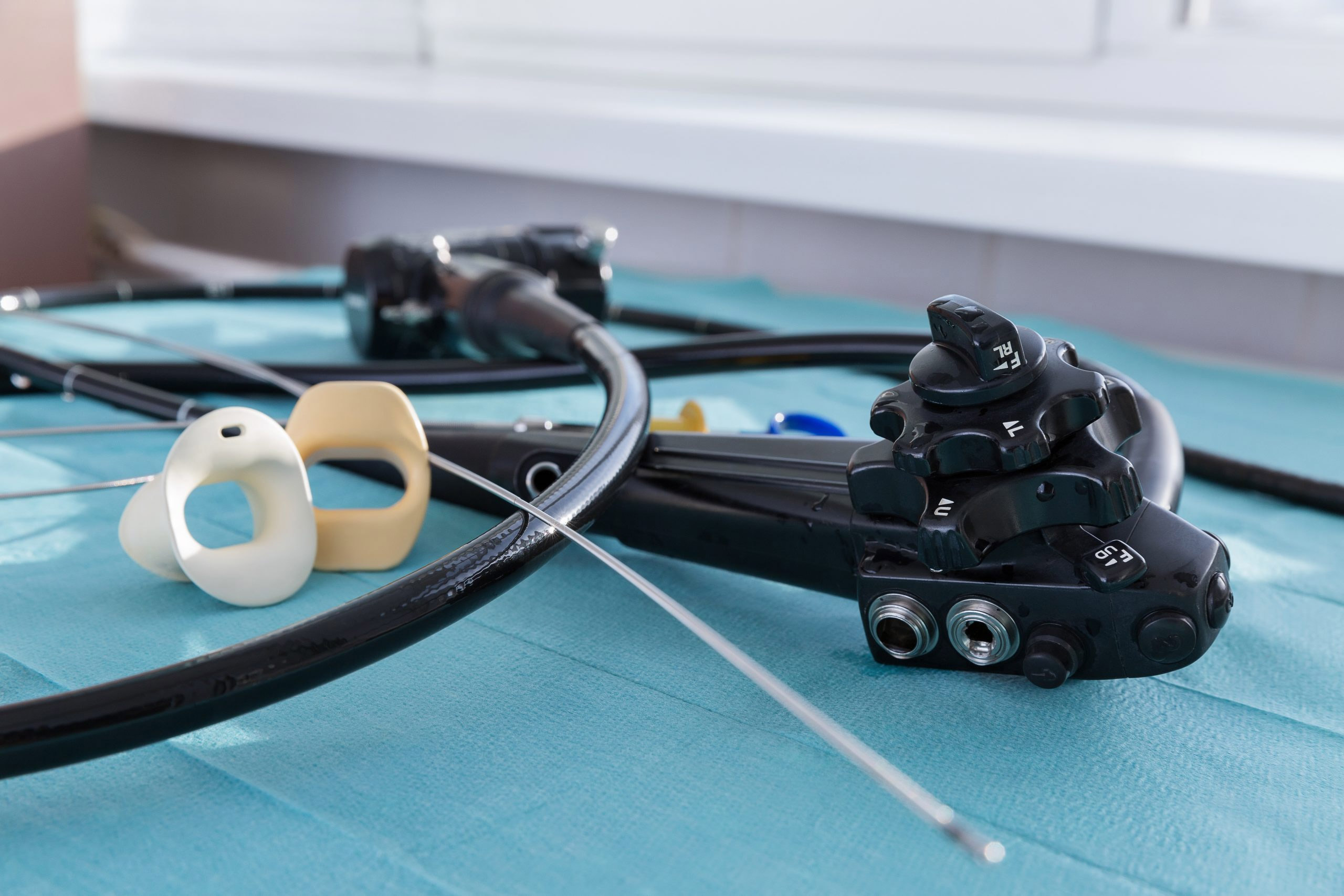
The five Burkholderia cepacia complex positive cultures were obtained from therapeutic and diagnostic urologic procedures, which had been performed by the same team in the same surgical suite. An investigation of the staff found no obvious infection control gaps and three flexible cystoscopes and one flexible ureteroscope were negative after culturing.
A process break, however, was reported in broth production protocol, where staff had added specimen to nonsterile saline to be used for blood bank use. The staff had also reused tubing and a spigot to access each new box of saline, which caused cross-contamination of each subsequent box. Additionally, reusable saline bottles were not cleaned routinely.
The protocol breach was determined to be related to two important factors: Staff was unaware saline obtained from the blood bank was nonsterile, and the saline setup in the blood bank was more convenient for after-hours staff. All specimens in question had arrived at the lab after hours because the procedures were done late in the day.
Among the corrections implemented after the investigation, nonsterile saline located in the blood bank is designated as such and is only to be used for blood typing. Each new bag of it also requires a new spigot.
“Organizational failures included the lack of policy awareness, education, and training for laboratory staff,” the authors write. “Technical failures included an ongoing lack of proper maintenance to items found within the blood bank including saline boxes, bottles, spigots, and tubing.”
Fortunately, the patients impacted by this pseudo-outbreak were unharmed and required no change in pre- or post-procedure antibiotic therapy. Outbreaks such as this, however, increase the risk of patient harm and may lead to unnecessary treatment, procedures, and healthcare costs, according to the authors.
They list four points of emphasis from the investigation:
Burkholderia cepacia complex is often resistant to common antibiotics. While it generally presents minimal risk to healthy individuals, it can be devasting to those with impaired immune systems or lung functions, according to the authors.
A previous outbreak of 71 patients developing Burkholderia cepacia urinary tract infections revealed another surprising source of infection: anesthetic gel used for lubrication and pain management.