Patients who underwent a cystoscopy procedure with a reusable scope had higher frequencies of post-operative encounters, urine cultures and hospitalizations, according to a recent Mayo Clinic study.
They were also more prone to experiencing “post-procedural 30-day encounters” — such as a phone call to the doctor, an emergency department visit or clinic appointment — directly related to complications arising from the procedure, researchers found.
Procedures performed with a single-use cystoscope demonstrated a lower incidence of post-procedure encounters and positive urine cultures.
The study’s findings were published in Urology Practice. The research underscores the significance of patient safety and efficiency optimization in medical procedures.
Dr. David Thiel, chief of clinical practice at Mayo Clinic in Jacksonville, Florida, talked more about the study’s findings in an interview with Urology Times.
Patients examined with disposable scopes had fewer engagements with the healthcare system, measured by metrics such as phone calls, urine cultures, and comparable rates of urinary tract infections and bladder tumor surveillance.
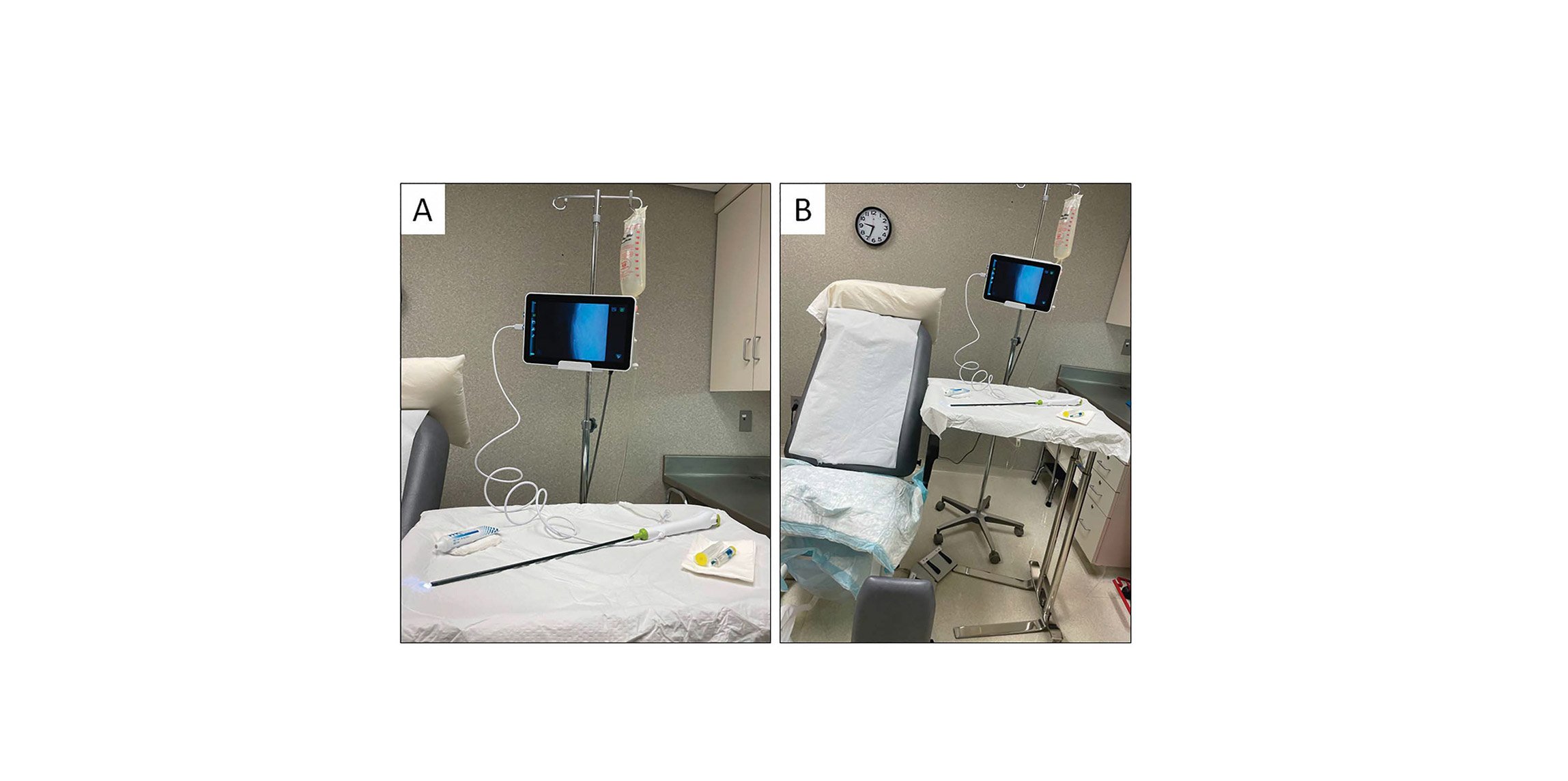
Recognizing the challenges involved in instrument reprocessing and repair rates, the urology clinic gradually transitioned to single-use cystoscopes, Thiel said.
Between June and September 2020, urologists at the Mayo Clinic conducted 506 cystoscopy procedures using cystoscopes that were reusable. The clinic carried out 494 procedures with single-use cystoscopes from February to May 2021.
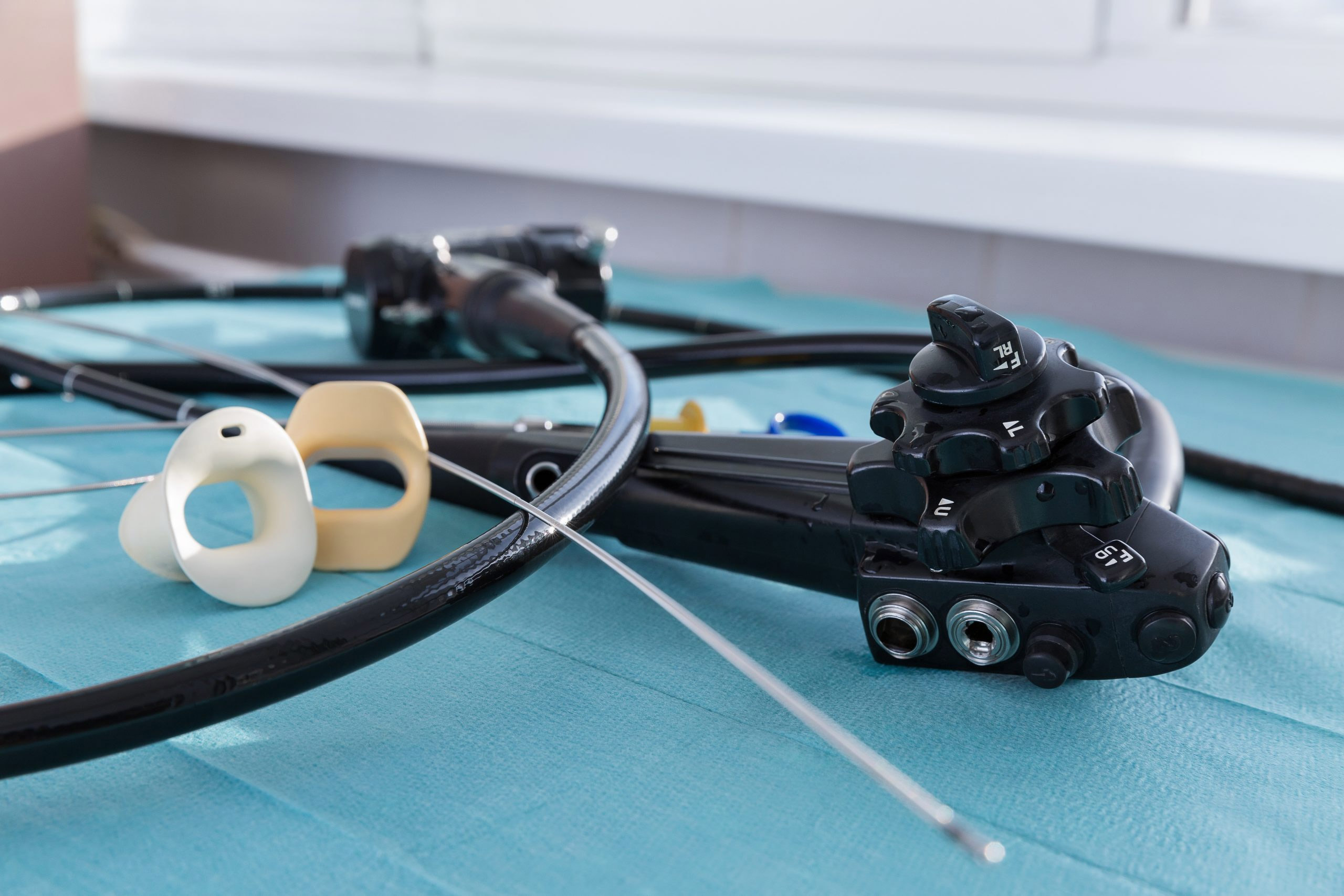
Concerns over endoscopy-related cross-contamination have gained media attention and FDA scrutiny in recent year. While rare, insufficient cleaning and disinfection practices have contributed to outbreaks, according to reports.
Single-use endoscopes help eliminate reprocessing and reduce cross-contamination risk.
When switching to single-use endoscopes, healthcare clinics should consider their impact on costs, infection rates, environmental impact, clinical workflow, and healthcare resource utilization, according to researchers.
Related: